Socializing with the ‘Insane’
After being admitted to the psych hospital, there is nothing to do except pace the hallway and swallow pills.
A better option for passing the time is socializing with other members of the ward community.
Inside the Community
“So, how did you get here?” I asked an unsuspecting peer on the ward. He was around my age and appeared somewhat approachable, speaking what I thought was sensible at first.
“Police brought me to CPAP… “he said with empty conviction. It was as if it had happened, but he didn’t know more about the story. Most peers can tell you ‘Why,’ instead of ‘how,’ they found themselves in an inpatient psych ward.
CPAP
CPAP is an emergency room but configured for psychiatric emergencies. So, when I asked why he was admitted, he told me not why but how. He left the most critical part providing little information about what was going on with him. The type of help the hospital would offer him and others.
Peers on the unit carry with them insight (or the lack of) and stories that can pass the time on days when you need to escape if only mentally, the confines of the unit. After so many hospitalizations, I have experienced the benefits and drawbacks of socializing with others in the hospital. Many specialized units and other specialized care settings target specific disorders and cater to a niche cross-section of the mental health community. Psychiatric units, like local restaurants, now cater to a particular client base, or diagnosis, when accepting new admissions.
These are memories helping to shape my understanding of my mental status on the unit. The better I understand these events the more I understand the help of the hospital.
Ah-ha! Moments
More interesting than how the system works are the stories of how they discovered themselves within an inpatient setting. Every person’s version of the precipitating events of their hospitalization is always fascinating. The most talked-about stuff on the ward–barn none- paints a picture of a peer with more humanity.
“Look!”. A patient gestured to her wrist, where She carved ‘HELP’ into her skin with scabs and stitches. Her skin was still red and irritated looking.
Understanding how minor problems become bigger is interesting on a clinical level. For her, help would mean feeling less pain. The hospital, for her, would deal with pain and help her find ways of soothing it and finding more comfort in her thoughts.
Why and How
The ward, or unit, sometimes feels like a place of healing and sometimes feels like jail. Depending on why and how someone gets there, their story will foreshadow their course of treatment. I like to think of it as socialization. After all, I’m talking with others on the unit, or getting to know the more significant peer community.
Similarly, there is an energy trial as patients pass through vitals and other triage areas on the unit toward their room and the patient regions. When a new patient sits down with everyone in the patient peer community or for their first meal, this is always a moment of anticipation, excitement, and total shock.
New Admissions
New admissions were ‘fresh meat.’ These patients are always at their peak, most disordered, and at a severe point in their illness. These folks seem always to leave a wake as a giant ship does to the surrounding water.
“Den of thieves!” exclaimed a patient. Wow, this is one bizarre situation and place I’m in.
Dirt and flowers were always falling out of her pockets on the floor. Even more strange, staff members constantly reminded Carol to stop taking ground from the flowerpots in her room.
Carol, or ‘Carol Flowers’, as she later referred to herself in writing, reminds me of the strange subtext that follows patients and new admissions.
First Admission
Given all the covert technical aspects around essential communication, it isn’t too hard to see that making friends on the unit can be highly complicated. My first adult admission was at age 20, at the peak of my development, a few months before I turned twenty-one. I was supposed to be at my graduation ceremony and graduate from Binghamton University.
Instead of attending graduation, moving up meant admission to the local hospital in Binghamton. If my situation wasn’t sad enough, I was transferred from the community hospital to the state after ‘failing out’ at the lower level of care.
As a college student, you could understand why I wasn’t familiar with this tiered system. I was puzzled as to why the same engagement skills I had just learned at one level of care weren’t working when I arrived at the state hospital. At the state level of care, patients seemed to be less responsive.
I still remember attempting to make conversation with a few people without any success before giving up. Most people had word salad or garbled language. “Banana, I’m tired”. Mumbled a peer, perplexing me ad nauseum. Unless a staff member was present, their speech was indecipherable. Most of them eventually fell off my radar until their speech cleared up. Or until I could make some sense of what they were trying to say.
Ground Floor of Dysfunction
People are so disordered that they cannot maintain a conversation without spinning out in tangents and non-sequiturs without end. God, damn! I thought, listening to her speak. Almost every other word was either out of sequence or misplaced. Except for one sentence, ‘I’ve been up and down this hill,’ remarking on her long relationship and rich history of hospitalizations on the hill, the local vernacular for the name of the hospital’s campus.
I wasn’t the only sick person who was hard to understand regarding essential engagement and communication. Depending on their diagnosis, other people encounter issues when holding a conversation. It was even more challenging to get someone’s entire picture for more extended, rawer, and more reflective discussions.
Life in the unit is full of dull moments. Sometimes, with all the silence, then just to be interrupted by treatment meetings and everyday team operations, it can be hard to put together with thought. New admissions to the unit offer a welcome break from the atmosphere.
Fresh Meat
Everyone usually gasps when the unit door opens and walks to a new admission, followed by an unmistakable pause. “Who is this?! What’s their diagnosis?” people ask each other every time a new admission hits the unit’s census.
Even before you could read the writing on the t-shirt, the newcomer was already slapped with a diagnosis. Everyone was eagerly waiting to greet the new admission.
New admissions to the unit are usually not healthy enough to engage in meaningful communication. In terms of approachability, many are still agitated. Making connections with other peers is a precarious venture in the hospital. It is almost impossible to know how socializing will pan out or benefit your situation.
Stories from newly admitted peers can and probably will be highly vivid, sometimes dark, and usually bizarre. “I am the lord’s anointed one, ready to usher in the age of judgment,” I distinctly remember hearing from a new admission.
At the same time, most people talk about their potential and future discharge. You may be lucky enough to catch someone in their low-level manic reflective mood talking about their feelings on how they ultimately needed the hospital. Reflection is followed by a litany of regrettable situations culminating in each patient’s ‘eye-opening’ admission. “That’s how I got here…” you would hear, repeatedly, with more or less insight each time.
Socializing in the Hospital
I have heard stories of all kinds, painted in both broad and sophisticated strokes depending on the mood, verbal acuity, or differing levels of self-disclosure.
One patient, Lady R. I got along with Lady R. well and spoke with her regularly. In Lady’s case, it seemed as if she was recovering. So, I invested my energy in speaking and connecting with her. I wanted to know what she was doing to experience some relief from her symptoms, whatever they were. I wanted to learn more.
One day, it seemed as if a switch had flipped. Suddenly, Lady was talking to herself again and responding to internal stimuli. One day, I noticed she was talking with hospital staff and pointing toward me. I was sitting on the couch in the day room at the time. I observed the team approach me and ask me what I was doing now.
“Max, one of the nurses, wants to speak with you.” One of the technicians advised me one day that speaking with her seemed to be not only tricky but troubling. I knew it! The other patient was complaining to the staff about me. She told the team that I was threatening her.
That was what the nurse told me later. I had to vouch for my behavior to the nursing staff. The staff believed me. After about a week, the team transferred Lady to long-term care.
In this case, I was entangled in Lady’s delusional system, and she reported it to staff. After looking into it, the team must have decided she was de-compensating and needed more help and stabilization than the admissions unit offered here.
Insightful Philosopher King
I have also met people so reserved, and seemingly together I wondered why they were in the hospital. I have one memory of a man interested in my writing from college. Days would pass, and I looked forward to walking beside this peer. We would talk about philosophy whenever we had the opportunity to converse.
I could relate to him. I could also speak without worrying he would make things even more difficult for me. After all, our general status, ‘mental status,’ was constantly being observed. I didn’t want to appear sicker than I was to be considered ready for discharge.
I couldn’t figure out why I was on the same ward as someone so healthy. As time unfolded, his behavior answered my questions.
The buzzer went off.
I heard screaming. Before I knew it, the staff called code.
Before I realized what was happening, the peer philosophy scholar was restrained.
I observed him as he lay flat on the crash cart, surrounded by staff. He had attempted to hurt himself.
Months passed, and he never returned to regular clothing. In his room, mostly isolated for my hospitalization, he remained in hospital clothing. For the rest of my time there, he appeared very depressed looking, and rarely gave me eye contact. The philosopher king certainly wasn’t behaving like the person I had met when I was a new admission to the unit.
The Yearbook
Upon discharge, my parents my family surprised me with a copy of my college yearbook they ordered prior to being hospitalized “It didn’t seem right to give it you earlier…” my parents said as they handed the school yearbook from Binghamton University.
I have several comments and signatures, including Carol Flowers and many others from people I socialized with in the psych hospital.
In the yearbook’s pages are inscribed their well wishes for me after moving on and discharge.
It was a space for their hope for a better future for me.
The inspiration, challenges, stories, and suggestions we get from socializing during difficult times (and good ones) will live on for another day. I hope it will persist far beyond the confines of the hospital. Let it aid you in reaching the upper limits of healing.
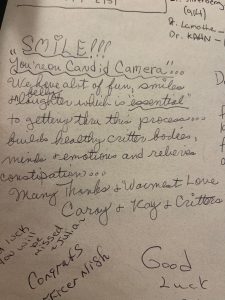
The accompanying photographs are the inside and front cover of my yearbook from 2008. The picture has random numbers, names, and good wishes. Centered in the photo is a note from ‘Cray Critters,’ one of the peers on the unit, talking about cameras taking secret photos–as in: ‘candid camera.’ The fonts are all different, with red and blue and black. “Good luck!!” is written in large lettering, with rounded edges and a blunted font.
The yearbook cover is green, with gold lettering, with “2008 Binghamton University” written on the spine.
Back to Top of Page | Back to Creative Nonfiction | Back to Volume 16, Issue 2 – Summer 2022
About the Author
Max E. Guttman’s battle with Schizophrenia began at Binghamton University in his last semester of college. Max was discharged from Greater Binghamton State Hospital Center in July of 2008 after spending six months there. His Recovery was swift, but not painless, and undoubtedly tricky—Mr. Guttman blogs daily on his site mentalhealthaffairs.blog. Mr. Guttman has published several journal articles on Recovery and mental health and four books: University on Watch, Small Fingernails, Wales High School, and Wales Middle School. Max is currently the chair of the C.A.B. committee (Consumer Advisory Board) for the Department of Mental Health and Hygiene in N.Y.C. Mr. Guttman’s primary responsibility is operating a private Mental Health practice, Recovery Now, L.L.C., conducting tele-psychotherapy.